Aspiration of Hematoma
Introduction
A hematoma is a collection of blood outside of a blood vessel. It usually occurs as a result of damage to the wall of a blood vessel wall, artery, vein or capillary, which leads to leaking of blood into nearby tissues. The hematoma may be tiny; containing just a dot of blood or it can be large and cause significant swelling.
The blood vessels in the body are under constant repair. Minor injuries occur routinely and the body is usually able to repair the damaged vessel wall by activating the blood clotting mechanism and forming fibrin patches. Sometimes the repair fails if the damage is extensive and the bleeding continues through the large defect.
Blood escaping from the blood stream can be very irritating and may cause symptoms of inflammation such as pain, swelling and redness. Symptoms of a hematoma depend upon its location, size and whether they cause associated swelling or edema.
Blood vessels which are fragile may contribute to hematoma formation. An aneurysm or weakening in a blood vessel wall may spontaneously leak.
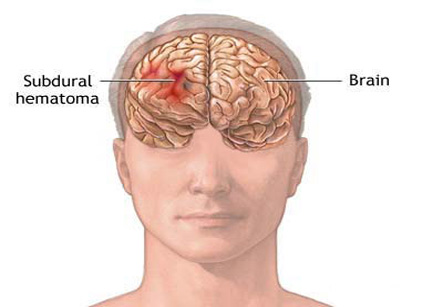
The medical term ecchymosis is commonly recognized as a bruise, or blood that has leaked out of a broken blood vessel under the skin. This injury is also called as contusion. An ecchymosis is usually flat while a hematoma has a three dimensional configuration. Hematomas may also occur in any organ and not just under the skin.
Trauma is the most common cause of a hematoma. The term trauma does not always mean car accidents, falls, head injuries, broken bones, and gunshot wounds, etc.. Trauma to tissue may also be caused by a trivial reason such as an aggressive sneeze or an unexpected twist of a limb. When a blood vessel is damaged, blood leaks into the surrounding tissue. This extravasated blood tends to coagulate or clot. The greater is the amount of bleeding, the larger the amount of clot formation.
The ear must be examined again for hematoma reoccurrence every 24 hours for several days.
There are many people who take blood thinning medications. These medications increase the potential for spontaneous bleeding and in turn for hematomas to expand. In this case, the body cannot efficiently repair blood vessels and blood continues to leak through the damaged areas.
Occasionally, some diseases may decrease the number of platelets in the blood stream (thrombocytopenia) or their ability to function. These platelets are the cells which help to initiate blood clot and fibrin formation.
All of the above situations may exist independently to cause a hematoma or they may occur in combination.
Hematomas of the skin and soft tissues, such as muscle and joints, are often diagnosed by physical examination alone.
Auricular hematoma can be considered as a prototype for drainage. This can be performed by using following technique:
Preparation
• The skin is cleansed with povidone iodine, chlorhexidine gluconate 2% and isopropyl alcohol 70%, or another cleanser.
• The area is anesthetized with lidocaine 1% or an auricular block may be performed.
Technique 1 – Needle aspiration
• This method is no longer recommended by many sources as it has a risk of hematoma re-accumulation. The aspiration is many times inadequate and the hematoma requires additional management. Some doctors recommend initial needle aspiration followed by the incisional method, if re-accumulation occurs.
• An 18- or 20-gauze needle is used to aspirate blood from the most fluctuant or full area.
Technique 2 – Incision and drainage
• The edge of the hematoma is incised along the natural skin folds using a scalpel. A small (about 5 mm) incision is often adequate.
• The skin and perichondrium is separated from the hematoma and cartilage. The hematoma is then completely expressed or suctioned.
• The pocket thus formed is irrigated with normal saline with an 18-gauzeangiocatheter.
• Optional method: A small drain is left in the incision. This allows the wound to drain but also predisposes to infection. If a drain is placed, the patient is always given a course of antibiotics upon discharge. The drain is removed in 24 hours if there is no significant bleeding.
• The perichondrium is then reattached to the cartilage.
Post-procedural care
• The ear must be examined again for hematoma reoccurrence every 24 hours for several days.
• Aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs), or anticoagulants should be discontinued or avoided for several days to prevent bleeding.
• The patient is always prescribed an antibiotic upon discharge to cover common skin flora for 7-10 days. Patients with weakened immune systems should receive antibiotic prophylaxis covering both Staphylococcus and Pseudomonas bacteria.
• If infections suggestive of Pseudomonas species are discovered during follow-up, the patient is admitted to the hospital for open drainage and started on intravenous antibiotics.